Maxim Rakovenko, an IT specialist from Tbilisi, Georgia, was only 35 years old when he was diagnosed with Hodgkin’s Lymphoma, a rare type of blood cancer. Just a generation ago, this would have been a death sentence in his country, which battled high rates of mortality after the collapse of the Soviet Union. Health care was inadequate because the market was highly fragmented, and doctors and nurses were insufficiently trained.
To rebuild its health-care infrastructure, the Georgian government privatized service delivery and introduced a basic universal health coverage (UHC) program in 2013. The private sector is now a key, collaborative partner with the government in the provision of services.
That gave Rakovenko the opportunity to be seen at an EVEX Polyclinic located in his neighborhood. The polyclinic provides a diverse range of services, with state-of-the-art medical equipment under the same roof. He started chemotherapy and radiotherapy treatment at a hospital that opened in March 2018. Half of the treatment cost was financed by Georgia’s UHC program. “The timely treatment conducted by a team of qualified doctors, coupled with the caring attitude of the hospital staff, helped me to recover,” says Rakovenko.
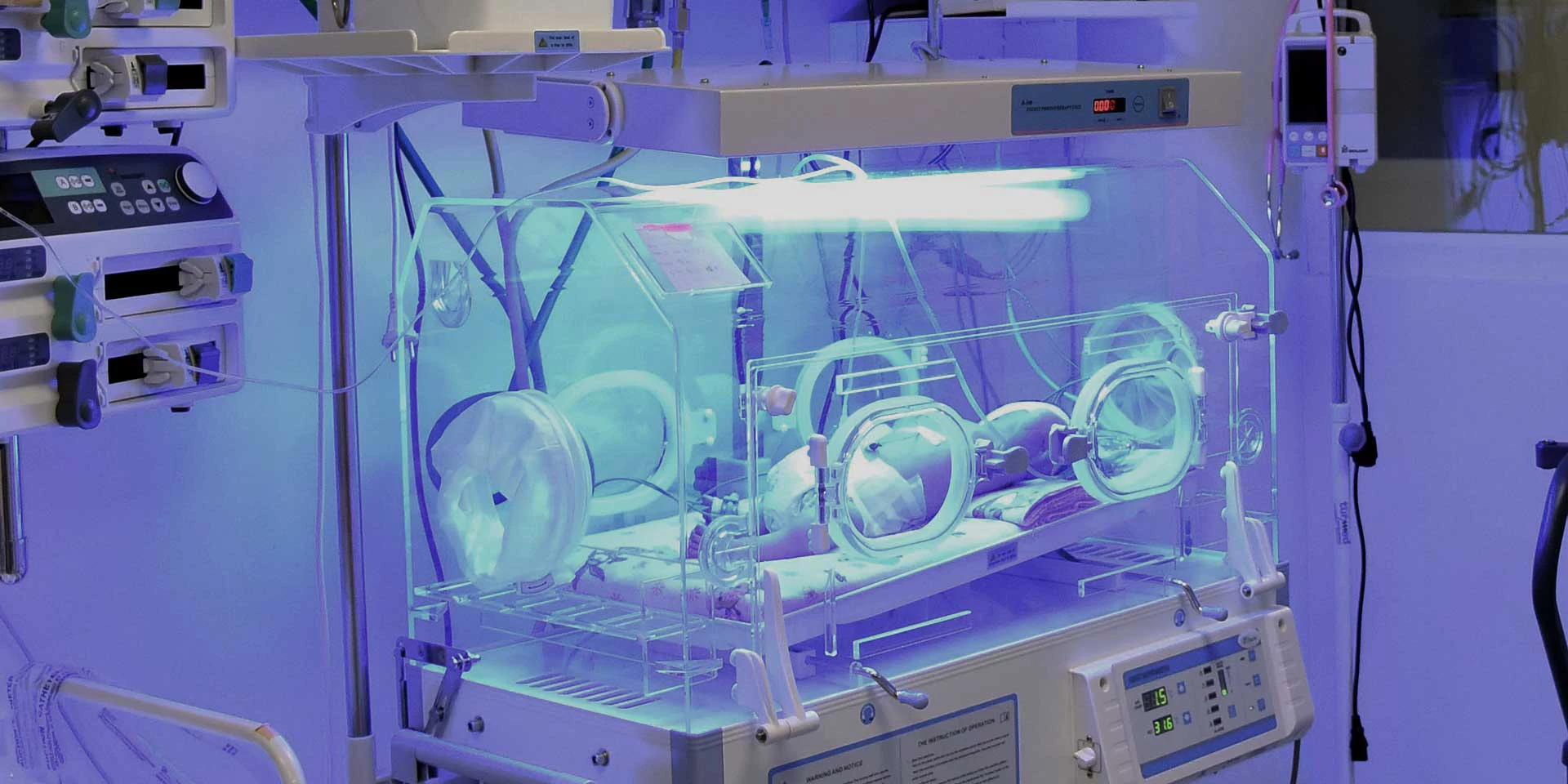
IFC helped, too—with a $25 million investment in EVEX’s parent company, the Georgia Healthcare Group (GHG). IFC supported the renovation of two hospitals acquired by GHG, expansion of outpatient services (like the polyclinic where Rakovenko had his first ultrasound), and introduction of new specialized services including pediatrics, cardiology, and oncology—some of which did not previously exist in Georgia.

GHG is now the largest employer in the country with about 15,500 full-time employees, including 3,600 physicians and 3,300 nurses. It is educating the next generation of doctors through 24 residency programs and is continually training its doctors, nurses, and other medical professionals in the latest techniques as it rebuilds the country’s medical workforce.
A Nationwide Prescription for Better Health Care
Although Georgia’s economy has been growing steadily in the past several years, high levels of income inequality persist, and roughly one in every five Georgians lives below the poverty line. Before UHC was introduced, many Georgians had been spending about one-third of their income on health care, while others were self-treating, or going untreated because they could not afford care.
That’s why UHC was rapidly embraced by people in Georgia. “With the introduction of a basic UHC program, equitable access to lifesaving treatment is now available to most of the population,” says GHG Chief Executive Officer Nikoloz Gamkrelidze.

UHC in Georgia is still funded by the public sector, but about 85 percent of care is delivered by the private sector. To administer this care, GHG has spent nearly $300 million in the last decade, upgrading Soviet-era facilities and building new hospitals and clinics with modern equipment. GHG is also improving services quality and patient safety by standardizing processes and working on implementation of international standards.
The continuing education for its doctors is a priority. Between 2015 and 2017 alone, GHG spent about $1 million per year training medical staff.
Cooperation Between the Public and Private Sector
The relationship between Georgia’s government and the private sector can offer lessons for other countries, despite the UHC program’s initial growing pains. Those started when UHC became so popular that it triggered budget overruns. The program was recalibrated to make spending more efficient, contain costs, and align expenses with what the government could afford.

The UHC model of cooperation in Georgia now provides the government and the private sector with significant benefits. Government can keep labor, pensions, and infrastructure build-outs and upgrades off the national balance sheet by shifting these expenses to the private sector. Private providers like GHG typically have lighter bureaucracy and greater motivation to deliver rapid results. For instance, GHG can overhaul hospitals in two to three years. This accelerates the timetable that governments can bring good care to market.
Private sector players, especially those with sufficient scale, can introduce western standards and roll out uniform, evidence-based care across the network. And they can benefit from accelerated growth, a reliable payment source, and increased scale and efficiencies.
Due to the size of integrated care networks, providers like GHG also have better bargaining power in purchasing disposables, non-medical supplies, medical equipment, and pharmaceuticals. These savings allow it to set prices in the average range—helping governments and citizens to spend scarce funds more effectively.
Join the conversation: #IFCimpact
Published in November 2018